Brain SPECT Info
WHAT ?
High Definition perfusion Brain SPECT (Single Photon Emission Computed Tomography) is a non invasive procedure which can detect functional changes by mapping the blood flow distribution, throughout the brain volume. In so doing it enables the description of abnormal features in the gray matter of both cortical and subcortical structures, based on the color rendition of relative perfusion maps.
HOW ?
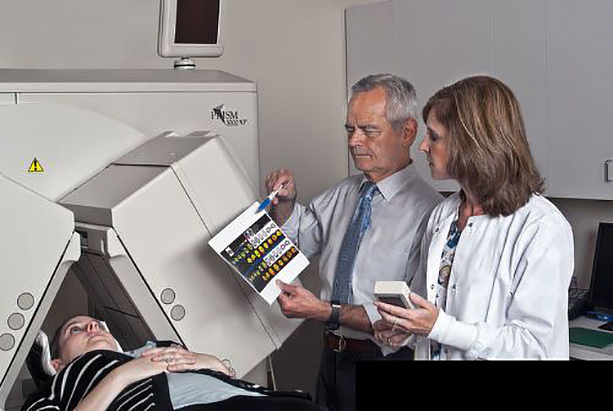
A molecule with special properties (HMPAO e.g. HexaMethyl PropyleneAmine Oxime) is labeled with a short lived (T1/2 = 6 hr) radiotracer (99m Technetium) and a small amount is injected intravenously under special surrounding environment conditions. Within 3 minutes this molecule is distributed in the gray matter in proportion to the blood flow which in turn is, in general, proportional to metabolism (the level of local gray matter activity). This distribution remains stable for several hours, which represents one of the major advantages of Brain SPECT. Subsequently the patient’s head is scanned, on a Gamma Camera, for an optimal number of minutes, while lying down in a comfortable position.
For the first two considerations one needs the best compromise between two factors: resolution and time of acquisition. This in turn, requires optimal technical specifications for the instrument used (the Gamma Camera) and, operational expertise.
There are several technical considerations when looking for a high quality Brain SPECT:
- Obtain as much structural detail as possible, which means acquiring a high information density (quality) study.
- Avoid head motion.
- Generate a superior quality display of the end product, which will enable a detailed report by the Nuclear Medicine physician (or other specially trained physician) and, in turn, facilitate the understanding by and the dialog with the referring physician. In addition this type of display can also be used to better ensure the patient’s own understanding and subsequent cooperation in the therapeutic strategy.
- Provide a detailed written report.
For the first two points one needs the best compromise between two factors: resolution and time of acquisition. This in turn, requires optimal technical specifications for the instrument used (the Gamma Camera) and, operational expertise as follows:
- High or preferably ultra-high resolution collimators which improve the definition of various anatomical structures and
- a triple head configuration which, minimizes the time needed for data acquisition.
- well trained and experienced Nuclear Medicine Technologists.
For the 3rd point, the key resides in high quality software and expertise which should enable the type of compelling, multifaceted, high definition , color and “user friendly” end-product display,which should accompany every report.
For the 4th point, the report itself, it should follow a sequential approach which looks and comments on all the anatomical features available, whether abnormal or not and concludes with the most likely symptoms / conditions (not necessarily diagnosis) correlating with the different abnormal features outlined in the text.
WHY ?
It is very common in the evolution of diseases affecting the brain gray matter that functional changes in metabolism / perfusion, occur long before a morphologic (structural) change can be detected by routine conventional brain imaging. This is especially true in Neuropsychiatry, where a High Definition Brain SPECT thoroughly interpreted by a specialized physician (Nuclear Medicine physician, or other Specialist specifically trained in Brain SPECT technique and interpretation) can help the referring physician tailor the medication to the particular individual patient (and shorten the workup duration in the process).
WHEN ?
The main indications are in complex cases with multiple co-existing conditions. This includes, for example, Neuropsychiatric disorders after head trauma, complex variants of epilepsy, more specific diagnosis and staging of CNS (central nervous system) degeneration (memory disorders, dementia, developmental disorders), cerebrovascular disease, attention and other learning disorders, affective disorders (depression, anxiety, bipolar disorder, OCD etc.), ADHD, neurotoxic effects of various etiologies including substance abuse, etc. and/or repeated treatment failures.
Brain SPECT is also used for following the evolution of a disease, evaluating prognosis and / or, for evaluating changes after treatment, or the lack of response to treatment. One general way to look at indications for Brain SPECT is to consider the empirical, frequent, real life situation briefly summarized in this sentence : “patient is symptomatic, diagnosis is unclear, and the morphologic exams (CT +/or MRI) are normal”. This is where Brain SPECT can often provide the additional insight needed for treatment planning. And finally a useful and very important reminder: Brain SPECT is a functional study!
WHERE ?
“A Brain SPECT, is a Brain SPECT, is a Brain SPECT” :
True or False ?
The fact that a Brain SPECT can be performed in many facilities does not mean at all that the benefits and information obtained are going to be equal. The decision about selecting the place to have a Brain SPECT done, can be simplified if the technical and expertise considerations, as mentioned above, are taken into account.
To summarize there is a need for :
- optimal instrumentation,
- optimized software
- well trained technologists and
- interpretational expertise.
The latter includes training, experience and, above all, a special interest and understanding of the underlying Neuroscience, Neuroanatomy and clinical questions addressed, as well as a close interaction between specialists (Nuclear Medicine , Psychiatrist, Neuropsychiatrist, Neurologist, Psychologist, Counselors, etc).
